Should the Use of Artificial Intelligence in Healthcare be regulated?
The use of artificial intelligence (AI) in healthcare has been growing at a promising rate. From disease diagnostics to drug development, personalization of treatment to gene editing, AI has led to many revolutionary healthcare transformations. In the near future, AI and big data are expected to provide more potential benefits for individuals and companies alike. A number of research studies have suggested that artificial intelligence can perform much better than humans at key healthcare tasks. However, given the technical and legal complexities associated with the field of medicine, there is a rising concern regarding the effectiveness of AI in medical practices. Patients still need protection from defective diagnosis, misuse of personal data and elimination of bias built into algorithms.
Types of AI Relevant to the Healthcare Industry
Artificial intelligence is an amalgamation of technologies, most of which have immediate relevance to the medical field, but the processes and tasks may vary widely. Here are some of the important technologies of high importance to healthcare sector.
Machine Learning
Machine learning algorithms process large data sets to detect patterns and execute tasks autonomously. In recent years, high availability of powerful hardware and cloud computing have resulted into a broad adoption of machine learning in different aspects of human lives. With the amount of data generated for each patient, machine learning algorithms in healthcare holds a great potential. From determining and labelling the kind of diseases to offering necessary medical information with accuracy, analyzing the patterns to predicting using current data and common trends, machine learning provide ample benefits to healthcare professionals.

The use of machine learning in healthcare has been around for a while but their adoption has become more widespread with the growing use of electronic record system and digitalization of various data points including medical images. One of the most important use cases of machine learning in healthcare is that it can be used to predict some of the most dangerous diseases at-risk in patients with the identification of signs and symptoms. During the COVID-19 pandemic, machine learning proved to be highly beneficial in determining the best sample for clinical trials, gathering more data points, analyzing the ongoing data, and reducing the data-based errors.
Physical Robots
Robotics have been undergoing massive transformation and tomorrow’s new innovations are expected to revolutionize the technology even further by creating intuitive healing. Medical robots are helping fill the gaps and transform the healing process for patients and caretakers alike. Nursing robots are helping out short-staffed teams by performing basic tasks such as drawing out blood or checking the vitals. For instance, a venipuncture robot can produce a 3D image of a patient’s arms to demonstrate nurses where the vein is, which makes the task of drawing out blood much easier. Sanitation robots are also being widely utilized for sanitizing and disinfecting healthcare centers. Assigning UV disinfection robots for cleaning, the maintenance workers will be able to focus on more important duties. Exoskeletons are completely transforming the healing process, especially for patients recovering from injuries that require intensive physical therapy.
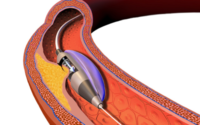
Micro robots are emerging as the next breakthrough in the robotics industry that have the potential to make surgeries less invasive and reduce recovery time. The microscopic robots are seamless enough to travel the human body performing repairs. So, the doctor would not require cutting open a patient for surgeries since the robots would be assigned the task. These micro robots are as small as single human cell and does not cause tissue damage compared to the conventional surgery methods.
Natural Language Processing (NLP)
Natural language processing is a sub-set of artificial intelligence that enables computers to interpret and understand human speech. The technology works by organizing data into a more logical format, breaking down into smaller semantic units or “tokens”. Optical character recognition is an NLP technique that scans unstructured data sets such as images or text files, extract text and tables from the data and present in a digestible format. Hence, OCR is commonly used to digitize clinical note, medical testes, history record, etc.
Robotic Process Automation
Robotic Process Automation (RPA) solutions prevalent in the healthcare industry are software that orchestrates other applications and performs tedious back-office tasks on their own. The intelligent software agents are ideal for process are ideal at processing transactions, manipulating data triggering responses, etc. The use of robotic process automation in medical insurance can lead to 30% reduction in claims processing costs. Infusing RPA in appointment scheduling and patient engagement software could eliminate manual data entry and improve no-show rates, which range around 5% to 39% depending on the healthcare institution. Leveraging robotic processing automation, medical organizations can facilitate processes without increasing labor costs, which constitute over 60% of hospital expenses, and accelerate labor-intensive tasks by 60%.
There is a growing need to strike a balance between setting guardrails for the AI and its associated technologies while allowing innovative ideas to flourish that can benefit the healthcare industry. Hence, FDA have acknowledged the rapid pace of innovation in the artificial intelligence, which can pose significant challenges.
How is FDA Regulating the Use of AI in Healthcare?
In January 2021, the FDA attempted to provide clarity on the introduction of artificial intelligence technologies in response to the rapid pace of innovation in the AI/ML medical device space. The FDA’s Center for Devices and Radiological Health (CDRH) has created a total product lifecycle-based regulatory framework for the utilization of AI that would allow for modifications to be made from real-world learning and adaptation. Besides, the regulations would also ensure the safety and effectiveness of the software as a medical device are maintained. Currently, the FDA reviews medical devices through pathways such as premarket clearance (510(k)), De Novo classification, or premarket approval. Depending on the significance or risk posed to patients, the FDA may also review and clear modifications to medical devices, including software. The FDA’s traditional paradigm was not designed for adaptive artificial intelligence and ML technologies.
The new regulatory framework could enable the medical device manufacturers to evaluate and monitor a software product from its pre-market development to post market performance. This approach could assure patient safety and improve the iterative improvement power of artificial intelligence and machine-learning based software. The new guidance includes a list of AI tools and technologies that can predict sepsis, identify patient deterioration, forecast heart failure hospitalizations, and flag patients addicted to substances.
FDA is also developing strategies to eliminate algorithmic bias, be it on the basis of race, ethnicity, or gender. For instance, pulse oximeter does not work on dark-skinned populations and some hip implants designed for female skeletal anatomy. These kinds of biases limit the efficacy of AI in real-world settings, as well as extent to which algorithms can learn and improve.
In the new regulations, FDA condemns manufacturers to include documentation to explain how the software used in algorithms works. The software details must include input data, image acceptance procedures, instructions provided to the users, interactions required by users in order for device to be used as intended.
FDA also cautions that manufacturers that quantitative imaging values from medical devices and imaging data can be affected by errors from a host of sources. The inaccuracies can result from systemic errors and random variations. Hence, understanding the source can enable manufacturers to measure quantitative imaging performance. Keeping track of the potential sources can help provide quality quantitative imaging results and determine all the potential areas where data could be problematic.