Manufacturing of Cell Therapies in the United States
The growing geriatric population and increasing prevalence of degenerative and chronic diseases have created a need for modern healthcare solutions that limit organ dysfunction and tissue degeneration. Regenerative medicine therapies focused on rejuvenation, regeneration, and replacement are changing how we think about medicine. Advances in cell therapies continue to be at the forefront of healthcare innovation, transforming how we treat and potentially cure certain diseases. These therapies utilize living cells to treat a variety of diseases, particularly those which currently lack any effective treatment option.
The advancement of therapeutic cell manufacturing has primarily been developed with a cell biology-driven approach, quintessential for the early development processes. As cell therapy matures scientifically and commercially, the pharmaceutical industry faces the challenge of creating safe, effective, and affordable products. Robust and standardized production of the cell therapies requires a high controlled manufacturing engineering strategy to increase batch consistency and efficiency.
Currently, the prices of cell therapies are high, mainly due to the labor costs, which account for around 50% of the cost of products used in the cell therapy manufacturing process. However, automation in cell therapy manufacturing has the potential to reduce manual intervention, which could significantly reduce the cost of cell therapy and adequately support commercial-scale production. The maturation of therapeutic technologies will also facilitate robust processes, improve product quality, and accelerate product delivery.
Types of Cell Therapies
- T-Cell Therapy
Chimeric antigen receptor (CAR) T-cell therapy is intended to genetically modify and program the body’s immune cells to find and destroy cancer cells. The CAR cells rely on stimulation signals inside the cell to do their job. With the gradual advancements in intracellular engineering, manufacturing one batch of CAR T cells takes less than seven days, which initially used to take several weeks.
- Stem Cell Therapy
Stem cell therapy stimulates the repair response of damaged or dysfunctional tissues with the use of stem cells or their derivatives. The synthetic stem cells are grown in a lab and manipulated to specialize into specific types of cells. The therapy is used to fight some types of cancer and blood-related disorders, such as leukemia, lymphoma, etc.
- Dendritic Cell Therapy
Dendritic cell therapy is a tailored cancer treatment vaccine made from our blood. Dendritic cells identify the body’s cancer as a threat and reintroduce new cells into the system to boost the system for combating against cancer. The monocyte-derived dendritic cells start with the isolation of monocytes from patient-derived peripheral blood cells using counterflow elutriation and controlled supplementation of cytokines.
- Natural Killer Cell Therapy
Natural killer cells are part of the innate immune system that respond to anything that appears to be a non-self, making them suitable for engineered cell therapies. Natural killer cells do not require to be genetically engineered to recognize cancer cells and are faster to prepare (less than 24 hours).
Clinical Trial Studies on Cell Therapy Manufacturing
Researchers and scientists in the pharmaceutical industry and academia have conducted more than 1200 cell therapy clinical trials in 2021 to develop robust techniques for creating novel products. Several kinds of regenerative medicines are starting to reach late-phase trials. Some companies are advancing CART T cell-based therapies to phase III trials for several indications such as HIV, immune deficiencies, and autoimmune disorders, and other conditions.
- Leukapheresis for CAR T-Cell or Adoptive Cell Therapy Manufacturing
Treatment of cancer patients with CAR T cells is one of the promising therapeutic approaches. Reproducible manufacturing of high-quality and clinical-grade CAR T cell products is essential for the broad application of the technology. Leukapheresis is the key to success for CAR T cell manufacturing. It is a procedure to segment white blood cells to make a special version of T-cells called chimeric antigen receptor (CAR) T cells. CAR T-cells have shown to be highly efficacious in eradicating a number of hematologic malignancies and thus predominantly used to treat refractory blood cancers. Despite the rapid transition from conception to commercialized therapy and significant development of processing technologies, CAR T cells have remained unchanged over the last 15 years.
Why is Automation Important for Cell Therapy Manufacturing?
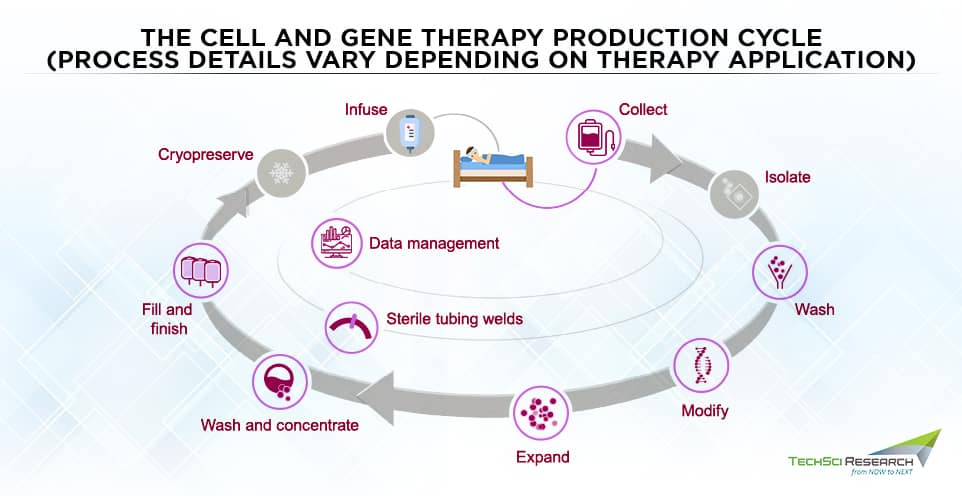
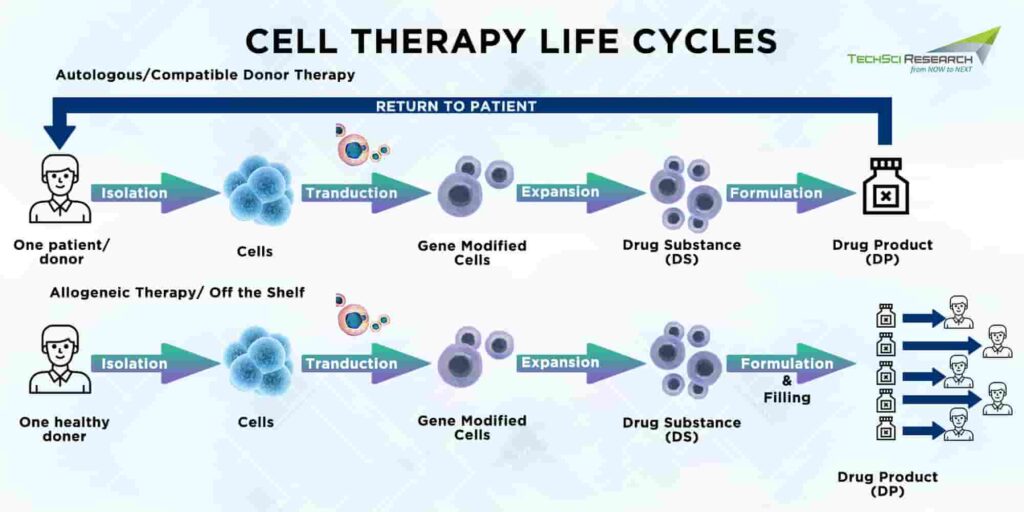
Cell therapy manufacturing starts with collecting cells from the patient and ends with the administration of the final drug product to the patient. Between the initial collection and final administration of the product, dozens of processes take place. Autologous cell therapies are personalized products thus, cell therapy manufacturers need to maintain the identity and ensure the chain of custody with every batch size. Almost all cell therapies are indicated for small patient populations, but automation and process simplification must be needed to meet the growing demands across multiple indications.
Manufacturing processes must move from open and manual to closed and automated to ensure greater product consistency and efficiency. The greater automation would also allow operators to measure certain critical attributes associated with the product and better control the variability of the starting material. Both industry and academia are already developing more automated, closed, and scalable systems to eliminate risks and scale up the manufacturing of cell therapies. Automation is particularly critical to assure low variability with less manual interaction. Timing is another aspect of automation to bring forward issues early on as efforts have to be duplicated if introduced too late.
Clinical Trials for Cell Therapy Manufacturing
More than 700 CAR T cells are under clinical trials. A significant challenge for the broader application of CAR T cell therapy is providing personalized therapy on a large scale. To overcome the limitation, there is a need to optimize lymphocyte collection through an improved leukapheresis collection process with the help of flexible and adaptable tools. Alternative methods of T cell collection are under investigation to minimize ex vivo manipulation to avoid contamination risks. Future research areas for cell therapy include non-CD19 targeted CARs, the ‘Sleeping Beauty’ technique for targeting B cell malignancies, CAR-transduced regulatory T cells for autoimmune disorders and haemophilia, and so on.
- Validation of a Process for the Manufacture of Stem Cells Isolated from the Nasal Cavity for Innovative Cell Therapy of Traumatized Peripheral Nerves
Faced with the limitations of surgical treatment, not much progress has been made in the quality of surgical treatment intended to repair damaged peripheral nerves. However, cell transplantation can be a perfect alternative for treating nerve damage, limiting inflammation, and improving axonal growth. Data gathered from studies suggests that mesenchymal stem cells are good cellular candidates for supporting nerve regeneration after transplantation as they exhibit high mitogenic activity and have a high potential for differentiation towards neural lineages.
The nasal ecto-mesenchymal stem cells are manufactured through the biopsy of a few cubic millimetres of the nasal cavity of adults taken during a surgical procedure. The cells taken from the nasal cavity are then amplified in vitro under pharmaceutical grade conditions and characterized for their ability to differentiate into neural cells. The cells are then cryo-preserved and thawed to validate and maintain their quality, proposing delayed implantation.
- Multicenter Trial of Stem Cell Therapy for Osteoarthritis (MILES)
Despite advancements in diagnosis and preventive care, any quest to develop disease-modifying osteoarthritis has proven unsuccessful. However, the mesenchymal stem cells can inhibit inflammation while promoting healing and thus help manage various ailments from cancer to genetic disorders. Autologous Mesenchymal Stem Cells (MSCs) therapy derived from the autologous bone marrow concentrate (BMAC) tends to heal the environment where it is injected. Thus, the BMAC mixture could aid patients suffering from osteoarthritis. Adipose tissue contains a large number of mesenchymal stem cells, and their cells are currently used in a variety of clinical studies within the regenerative medicine field.
Cell Therapy Manufacturing Patents
The rise in demand for cell-based therapies for the treatment of a variety of health conditions as well as a growing number of innovative products and new technologies have resulted in an increasing number of patent applications and grants of patents in recent years. Robust cell-based therapies need to be legally protected the same way as conventional small-molecule drugs. However, patenting a biological product comes with obstacles. Many characteristics of the biological-based products may weaken or limit patentability, such as inherent complexity and patient specificity.
Additionally, many biological products are considered “products of nature” and, therefore, not patentable as human made innovations. Some therapies may not be provided with patent protection, which is generally available for small-molecule drugs. Despite strict regulations for patents in the United States, many companies and educational institutions such as Novartis AG, University of California, F. Hoffman La Roche, University of Texas, Harvard College, Massachusetts Institute of Technology, etc. have been successful in patenting their cell-based therapies. Juno Therapeutics Inc filed the most patent applications in 2021 and became the top patent owner of the cell-based therapies in 2021.
Cell therapies have been commercialized in the United States with the launch of autologous chimeric receptor T-cell therapies such as Kymriah and Yescarta. Novartis relinquished a patent granted for its promising new gene therapy for certain forms of leukemia, known as Kymriah. The cell therapy is one of the first promising treatments to receive patent approval in Europe. Kymriah is specifically designed for treating relapsing forms of acute lymphoblastic leukemia. Novartis CAR T cell therapy involves collecting a patient’s T cells and genetically modifying and reinfusing them into the patient’s blood to target cancer cells more effectively. Kymriah is one of the most popular treatments for cancer, and more similar therapies can be expected to enter the healthcare domain in the near future. Hence, patentability of such a procedure is essential for setting a precedent.
With the advent of more such innovative therapies, patent applications have increased multi-fold to avoid any kind of dispute. Leading drug therapy for blood cancer, Yescarta CAR T drug, whose patent was owned by Bristol-Myers’ Juno Therapeutics and Sloan Kettering Institute for Cancer Research was announced invalid by the US Court of Appeal for Federal Circuit due to lack of “substantial evidence”. Gilead Sciences manufactures Yescarta for the treatment of certain types of large B-cell lymphoma and a jury ruled that royalties on the sales of the drug must be paid to Bristol-Myers in 2019. Gilead won USD1.2 billion for the reversal of Bristol-Myers decision and the dispute over revolutionary technique came to an end in 2021.
Way AheadAlthough cell therapy is continuing to change the lives of cancer patients, many of these therapies are still under the research and development phase. While many current cell therapies are primarily focused on oncology, the curative potential of cell therapies is being explored for a range of autoimmune and inflammatory disorders. Furthermore, the expansion of cell therapy technologies will be critical for the therapies to reach their full clinical and commercial potential.



